Background of the Federal Health Agency Overhaul
The recent announcement by the Trump administration to dramatically restructure the U.S. Department of Health and Human Services (HHS) has set off a wave of mixed feelings and heated debate. In an effort to streamline operations and cut bureaucratic sprawl, the administration plans to slash 20,000 full-time positions within the sprawling agency—a move that promises to reshape the federal health landscape in ways that many believe could have long-lasting impacts on public health in the United States.
At its core, the reorganization is designed to trim the agency’s workforce from approximately 82,000 to just 62,000 employees. To achieve this, the government intends to combine cuts made through early retirement packages, the controversial “Fork in the Road” offers extended to employees, and an additional reduction in force (RIF) that aims to remove 10,000 more positions. This sweeping decision is coupled with a significant restructuring within HHS’s various divisions, reducing the number from 28 distinct parts to only 15.
In the wake of this announcement, HHS Secretary Robert F. Kennedy Jr. defended the plan, claiming that the changes would not only curb what he described as a “dysfunctional, sprawling bureaucracy” but also realign the agency with what he identified as its core mission—reversing the chronic disease epidemic. While his comments have been met with fervor by supporters, critics from across the political spectrum have raised concerns about the potentially overwhelming, tricky parts of executing such a far-reaching overhaul.
Detailed Breakdown of Job Cuts and Department Reorganization
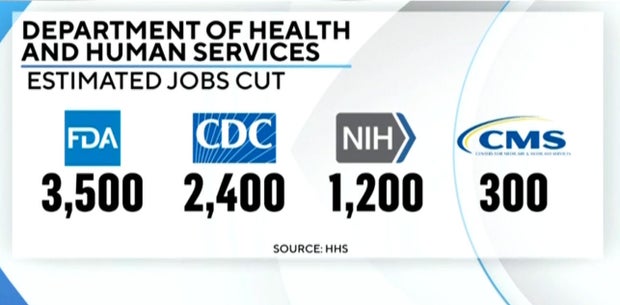
The proposed job cuts and departmental consolidation are two sides of the same coin. The high-level decision-making involves a blend of financial prudence and a fundamental reevaluation of what roles within HHS are considered essential. The following table summarizes the announced reductions by agency:
| Agency | Number of Jobs Affected |
|---|---|
| Food and Drug Administration (FDA) | Approximately 3,500 |
| Centers for Disease Control and Prevention (CDC) | Approximately 2,400 |
| National Institutes of Health (NIH) | Approximately 1,200 |
| Centers for Medicare & Medicaid Services (CMS) | Approximately 300 |
In addition to these numbers, there is an undisclosed mix of employees from the “Fork in the Road” program and those inclined to take early retirement, adding up to further reductions. The administration asserts that these combined cuts will generate an estimated $1.8 billion in savings—a figure that, while important on paper, raises many questions about the potential trade-offs in terms of public safety and effective regulatory oversight.
Moreover, one of the most controversial elements of the plan is the creation of the Administration for a Healthy America (AHA). Intended to consolidate various agencies within HHS, the AHA will focus on coordinating programs that deal with chronic care and disease prevention. Areas such as primary care, maternal and child health, mental health, and HIV/AIDS virus prevention are pointed out as key priorities. Yet, the planned new structure prompts concerns over the potential loss of specialized focus, as the creation of one giant umbrella organization might obscure some of the subtle details that make each existing agency effective in addressing its particular mission.
Assessing the Reactions: Politicians, Employees, and Public Opinion
There is little doubt that the restructuring has stirred strong feelings both within and outside the HHS. Politicians from different parties have voiced their perspectives, ranging from staunch approval to outright condemnation.
Supporters Praise the Streamlining Efforts
Advocates for government efficiency—including those who appreciate a leaner federal structure—have welcomed the initiative. Some argue that the cutting of seemingly redundant positions and excessive layers of bureaucracy will help make the federal government more responsive to current challenges. On social media, notable supporters have highlighted the financial efficiency of the plan, with one prominent figure from the pro-efficiency movement stating, “The insane spending and staffing in healthcare is actually the cause of our bad health outcomes.”
Critics Warn of Overwhelming Consequences
On the other hand, critics warn that the creation of “little fiefdoms” within HHS could lead to a worrying reduction in critical oversight functions. Figures like Sen. Angela Alsobrooks (D-Md.) argued emphatically that the proposed mass layoffs are “dangerous and deadly,” citing that such comprehensive cuts could impair patient protections and oversight mechanisms essential to preventing fraud and abuse.
In addition to political figures, frontline staff within key agencies such as NIH have expressed their apprehensions. Reports from anonymous employees reveal that not only is there a palpable sense of exhaustion and fear for personal job security, but also a concern that the reset could lead to a diminished ability to fulfill the agencies’ missions. One NIH worker commented on the nerve-racking uncertainty, noting that many staff members feel that the reductions could leave the remaining employees with a heavier workload and decreased support. This sentiment is echoed throughout the internal discussions at HHS.
Evaluating the Impact on Public Health Oversight and Services
The restructuring of HHS presents a myriad of tangled issues when it comes to public health oversight. Many are questioning whether consolidating divisions and cutting thousands of jobs might lead to a cascading effect on the quality of the supervision over public health programs. Similar concerns have been raised about the timing of moving the Administration for Strategic Preparedness and Response (ASPR) under the CDC – a change that some worry could diminish its capacity to respond quickly to natural disasters and health emergencies.
Key Areas of Concern in Public Health Services
- Regulatory Oversight: With fewer inspectors, reviewers, and oversight officials in place, there is concern that the FDA and other agencies may not effectively catch mistakes or fraudulent activities. The cuts promise to spare drug, medical device, or food reviewers, but the overall loss in administrative support might lead to slower response times to emerging issues.
- Response to Emergencies: The shift of ASPR under the CDC could affect its broad emergency-response mandate. Former ASPR executives have warned that this reorganization might limit the agency’s scope, hindering its ability to deploy resources quickly during crises.
- Support for Chronic Care: The consolidation of departments into the Administration for a Healthy America brings into focus the management of chronic diseases—a persistent challenge. Supporters assert that a streamlined structure would allow for better coordination of care. However, critics worry that such large-scale reorganization could disrupt service delivery in the short term, leaving vulnerable populations at risk.
Each of these areas is riddled with challenges that demand a careful, nuanced approach. The fine points—aspects that might seem like mere little details at first glance—are, in reality, the building blocks of a robust public health system. Losing touch with these subtle parts could compromise the entire structure.
The Delicate Balance: Financial Savings Versus Public Service Outcomes
One of the central arguments made by the administration is that the cuts will save nearly $1.8 billion while simultaneously reducing government waste. In theory, a leaner HHS should be more agile and better aligned with modern healthcare challenges. However, the reality of such drastic measures comes with potential pitfalls.
Cost-Cutting Measures and Their Hidden Complexities
When evaluating savings derived from job cuts, it is important to consider the following points:
- Short-Term Gains vs. Long-Term Costs: While immediate savings might appear attractive, long-term consequences—such as increased inefficiencies, greater wastage, or even health emergencies—could offset these financial benefits.
- Impact on Workforce Morale: Extensive cuts could lead to an overwhelming number of remaining employees being saddled with extra responsibilities. When a workforce is already facing nerve-racking uncertainty about job security, this additional stress could hamper productivity and overall public health service delivery.
- Innovation and Collaboration Risks: A reduction in administrative layers might provide a leaner workflow, but it could simultaneously stifle the opportunities for innovation and cross-agency collaboration that are critical to addressing complex health challenges.
These points underscore the necessity of finding a path that balances saving taxpayer money with maintaining an operational, responsive health administration. The process of sorting out these issues involves a careful examination of both the immediate benefits and the long-lasting outcomes that such a restructuring might bring.
Comparing Past and Present Approaches to Health Administration
Historically, HHS has been known for its size and its broad scope, encompassing an array of agencies like the CDC, NIH, FDA, and CMS. Each of these bodies has its own culture, specialized functions, and set of challenges. The current restructuring represents a significant departure from decades of established practice, where specialization and inter-agency coordination were key to the country’s approach to public health.
Then and Now: A Comparative Look
| Aspect | Traditional Structure | Reorganized Structure |
|---|---|---|
| Number of Divisions | 28 distinct parts | 15 consolidated divisions |
| Total Workforce | Approximately 82,000 employees | Approximately 62,000 employees |
| Management Style | Decentralized with strong agency specialization | Centralized with integrated oversight functions |
| Budget Allocation | Heavily focused on Medicaid, Medicare, and research funding | Aiming to balance cutbacks with strategic reallocation |
This table illustrates the major shifts that are taking place. Proponents of the change argue that consolidating agency functions under a unified strategy will allow HHS to streamline processes and shed unnecessary administrative overhead. However, detractors remain skeptical that such a dramatic restructuring can maintain the same level of detailed oversight when many of the traditional, small distinctions that separated agencies are being blurred.
Concerns Over Workforce Morale and the Future of Scientific Research
Beyond policy debates and administrative restructuring, there is a palpable human element in this story. Federal employees—especially those at the NIH—are expressing deep concerns about what these cuts mean for their job security and the future of scientific inquiry in America. For many researchers, the newly announced reductions are feeling like a heavy blow to the long-established culture of research excellence that has defined the NIH over the decades.
Employee Anxiety and the Potential Impact on Research
Several key points mark the general sentiment among federal health workers:
- Job Uncertainty: With thousands of positions under threat, the anxiety among employees is palpable. Workers are not only worried about their own futures but also about the potential loss of experienced personnel who have deep knowledge of the system’s complicated pieces.
- Productivity and Efficiency Concerns: The fear is that remaining staff members will be overburdened with additional responsibilities, leading to delays, burnout, and an overall impact on the efficiency of public health services.
- Impact on Scientific Discovery: NIH employees worry that a reduction in administrative support, coupled with diminished workforce morale, might slow down critical research projects. This, in turn, could hinder medical breakthroughs and slow the progress of treatment discoveries.
All these points combine to paint a picture of an agency at a crossroads, faced with the challenge of balancing cost efficiency and operational effectiveness with the need to remain a world leader in medical research and innovation.
Assessing the Impact on Emergency Preparedness and Disaster Response
Another crucial piece of the puzzle is how the restructuring may affect emergency preparedness and the rapid deployment of resources during health crises. The decision to reposition the Administration for Strategic Preparedness and Response (ASPR) under the CDC has sparked debate among experts who caution that such a move might restrict the scope of ASPR’s capabilities.
Emergency Response: Potential Gains and Pitfalls
The main issues at play include:
- Integration Versus Autonomy: Supporters argue that aligning ASPR with the CDC could lead to better coordination during infectious disease outbreaks and other emergencies. However, detractors are concerned that this integration might diminish the agency’s autonomy, limiting its ability to respond effectively to non-infectious medical emergencies.
- Learning from the Past: Lessons learned during the COVID-19 pandemic suggest that a quick, agile response is critical. Former ASPR leaders have voiced concern that the reorganization might result in nerve-racking delays or miscommunications during a crisis.
- Resource Allocation: With fewer resources and a leaner management structure, the integrated ASPR may struggle to maintain the same level of preparedness that was seen under a more dedicated, independent structure.
These points emphasize the intricate balance that must be struck between administrative efficiency and the need for rapid, robust emergency response capabilities. As the nation continues to recalibrate its approach to public health in a post-pandemic era, it is off-putting to consider whether these structural changes could compromise the agility that many experts feel is critical for emergency management.
Government Efficiency Versus Public Health: A Tense Balancing Act
The restructuring of HHS is a clear example of the tug-of-war between the drive for greater government efficiency and the imperative to provide high-quality public services. While the plan is heralded by some as a necessary step to curb wasteful spending and reduce bureaucratic overreach, many fear that the move could have unintended, negative ripple effects across the entire health system.
Key Perspectives on Government Efficiency
Examining both sides of the argument reveals several key considerations:
-
Efficiency Advocates Claim:
- The consolidation of agencies will reduce overlapping responsibilities and enhance coordination.
- Taxpayer savings can be redirected to more effective public service initiatives.
- A leaner workforce can potentially lead to more innovative approaches to resolving public health challenges.
-
Critics Counter:
- Significant job cuts may remove essential checks and balances that prevent fraud and ensure effective healthcare delivery.
- Loss of specialized support could lead to slower decision-making and compromised regulatory functions.
- The morale of remaining employees may suffer, ultimately reducing the overall quality of public service.
Ultimately, it is essential to recognize that any attempt to find your way through these tricky parts of administration reform must reconcile the genuine need for efficiency with the equally critical necessity of maintaining robust public health oversight.
The Hidden Economic and Social Implications of Health Agency Downsizing
The downsizing of HHS does not exist in a vacuum—it carries significant broader economic and social ramifications. While supporters focus on the financial savings and potential for reallocation of resources, critics highlight the possible long-term consequences that might hamper the nation’s overall economic resilience and public well-being.
Economic Considerations
Financial implications of the restructuring include:
- Immediate Savings: The projected $1.8 billion in savings could be seen as a boost to government finances. However, such savings might come at the cost of additional long-term expenses if public health crises become more expensive to manage due to reduced oversight.
- Workforce Disruption: Losing a significant segment of the federal workforce is bound to have ripple effects in local economies. With thousands of employees potentially out of work, there may be a slowdown in spending that could impact community businesses and local services.
- Innovation Impact: Reduced government backing for research could have knock-on effects in associated industries, limiting the country’s capacity to lead in groundbreaking medical research and technological innovation.
Social Considerations
On the social front, there are several aspects that warrant attention, including:
- Public Trust: Changes in federal health agencies can be nerve-racking for the public, especially if they believe these cuts will compromise the quality of care or the ability to quickly detect and respond to health emergencies.
- Community Health Outcomes: The reorganization might lead to gaps in services, ultimately affecting the health outcomes of vulnerable populations who rely on government-funded programs for critical care.
- Political Ramifications: The debate surrounding these cuts is highly loaded with political tension. As both sides use charged language to defend or criticize the changes, there is a risk that public policy could be driven more by partisan divides than by a clear-eyed assessment of what is best for public health.
In sum, stripping away thousands of jobs in a bid to cut costs may yield short-term financial benefits, but the long-term social and economic costs cannot be underestimated. A strategy that appears straightforward on the surface is, in fact, riddled with tension and hidden issues that must be carefully considered.
Future Implications: Charting a Path Forward
The restructuring of HHS is an unfolding issue with consequences that may reverberate through years to come. Both government officials and public health experts are now tasked with the formidable job of sorting out which adjustments will prove beneficial and which might lead to unintended setbacks.
Key Areas to Watch in the Coming Months
-
Implementation of New Structures: How the Administration for a Healthy America is integrated with existing agencies
will be a critical point of observation. Will it truly enhance coordination, or will it further complicate the already tangled issues of federal oversight? - Employee Adaptation: The workforce’s response to the cuts, both in terms of maintaining morale and adapting to new roles, will likely determine the overall efficacy of the change.
- Public Health Outcomes: Ultimately, the success of these reforms will be measured by their impact on public health—ranging from the speed of emergency response to the efficiency of regulatory oversight.
- Budget Reallocations: With nearly $2 trillion at its disposal, the budgetary shifts within HHS must be managed carefully to avoid compromising vital services such as Medicare and Medicaid.
As the nation embarks on this new chapter of health administration reform, it will be crucial to keep a close eye on these areas. Policymakers and health professionals alike must work together to ensure that in their attempt to reduce costs, they do not inadvertently sacrifice the quality of public health services—a consideration that is super important for all Americans.
Looking Beyond the Reorganization: The Broader Debate on Federal Government Size
In many ways, the HHS restructuring is a microcosm of a larger, ongoing debate in American politics: how to balance government efficiency with robust public services. Proponents of a minimalist federal government argue that leaner operations allow for faster decision-making and cost savings. At the same time, critics maintain that reducing the number of employees and the degree of regulatory oversight could lead to a decline in service quality and greater risks for public health.
The Underlying Issues in the Debate
Some of the key issues include:
- Responsiveness versus Stability: Supporters believe that less bureaucracy translates into a more nimble government capable of responding quickly to emerging health crises. Conversely, detractors argue that those extra layers of oversight provide critical stability and accountability.
- Cost Savings versus Service Delivery: There is a thin line between cutting wasteful spending and undermining the systems that ensure quality healthcare. In this regard, every cut might save money in the short term but could result in nerve-racking outcomes if essential services are compromised.
- Short-Term Restructuring versus Long-Term Impacts: While administrative reorganization can appear attractive in the immediate wake of budget concerns, it is the long-term consequences—which may include diminished innovation and critical oversight—that raise red flags for many experts.
This foundational debate is set to continue as the reorganization unfolds, providing a fertile ground for further discussion among policymakers, healthcare professionals, and the general public alike. In the meantime, both sides must strive to figure a path through what will undoubtedly be a challenging transition.
Concluding Thoughts: Balancing Efficiency, Oversight, and Public Trust
The Trump administration’s decision to reorganize HHS by slashing 20,000 jobs and consolidating its divisions sets the stage for a dramatic transformation in federal public health management. As the changes take root, it is essential to remember that policy decisions of this magnitude come with twists and turns that extend far beyond mere cost savings. While a leaner government may offer the promise of reduced waste and a more agile regulatory framework, the potential fallout—from employee uncertainty to reduced oversight and, ultimately, compromised public health—cannot be overlooked.
The reorganization reflects a broader ideological shift that champions government efficiency over longstanding bureaucratic traditions. Whether this change will bring about more effective healthcare delivery or create a host of new, confusing bits remains to be seen. As public debates continue and the full impact of the restructuring begins to manifest, one thing will be clear: finding the right balance between cost-cutting and service quality is a nerve-racking challenge that demands careful scrutiny, energetic debate, and ongoing evaluation.
For now, the nation watches closely as HHS embarks on a journey of profound change—a journey marked by significant reallocation of resources, redefined priorities, and a commitment by some to create a more streamlined government. The coming months will be crucial in determining whether these changes will lead to a more efficient and responsive healthcare system or whether they will compromise the very foundations of public health oversight that many Americans rely upon.
As we step forward into this new era, it is our collective responsibility to dig into these issues, hold our leaders accountable, and ensure that the promise of a leaner, more efficient government does not trample the essential services that underpin our health and well-being. In the end, the goal must be to protect and enhance the safety, health, and prosperity of every American—a mission that remains as super important now as it has ever been.
Originally Post From https://www.kawc.org/npr-news/2025-03-27/the-trump-administration-restructures-federal-health-agencies-cuts-20-000-jobs
Read more about this topic at
Massive Shakeup: Health and Human Services to Lay Off …
RFK Jr. plans to slash HHS workforce by 25% in massive …


